On October 17th, 2023, I had the incredible opportunity to attend a presentation titled “Nutritional Psychiatry for the Prevention and Treatment of Mental Disorders” by Professor Felice Jacka OAM. Professor Jacka is a renowned expert in the field of Nutritional Psychiatry, and she serves as the director of the Food & Mood Centre at Deakin University. She is also the founder and president of the International Society for Nutritional Psychiatry Research. Notably, Professor Jacka’s pioneering work has established the critical connection between diet and its influence on common mental disorders, positioning diet as both a risk factor and a treatment target.
During her enlightening talk, Professor Jacka highlighted extensive evidence that supports the links between diet quality and brain health, transcending countries, cultures, and age groups. She emphasized the immense potential for clinical and public health interventions centered around nutrition to prevent and treat mental, neurodevelopmental, and neurodegenerative disorders. She shared insights from existing research and discussed ongoing studies and initiatives conducted at the Food & Mood Centre.
Furthermore, Professor Jacka delved into the critical issue of our current global food environments and the transformative impact of Nutritional Psychiatry on policy and clinical guidelines. Her influence in the field extends far and wide, with her research and expertise cited in over 100 policy documents, including those of prestigious organizations like the WHO and UNICEF. In recognition of her remarkable contributions, Professor Jacka was awarded a well-deserved Medal of the Order of Australia (OAM) in 2021 for her dedicated services to Nutritional Psychiatry.
I would like to extend my sincere appreciation to the organizers, the Nutrition Society of Australia and the University of South Australia, for making it possible for us to meet and learn from Professor Felice Jacka, a true trailblazer in the realm of Nutritional Psychiatry.

What is nutritional psychiatry?
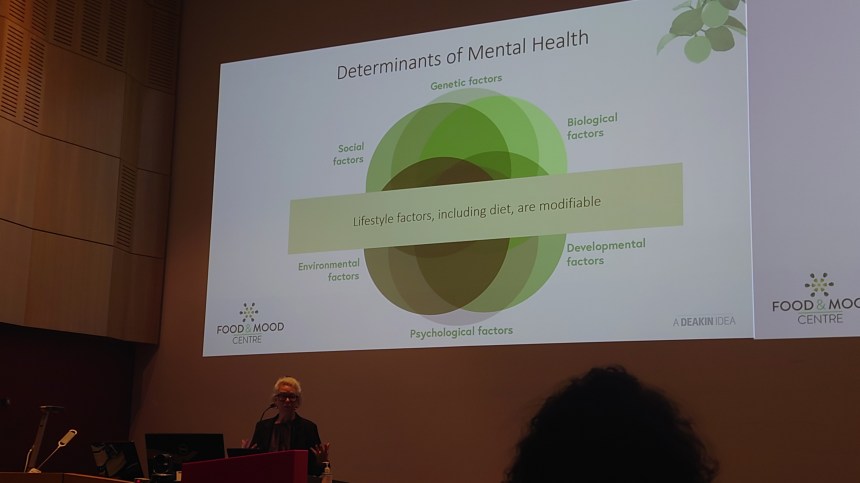
Nutritional psychiatry is an emerging field of study that focuses on the relationship between diet and mental health. It explores how the foods we eat can influence our mental well-being, emotional state, and cognitive function. The central idea of nutritional psychiatry is to investigate and apply evidence-based nutritional approaches to the prevention and treatment of mental and brain disorders, as well as their comorbidities (co-occurring health conditions).
Here are some key points related to nutritional psychiatry:
- Global Burden of Poor Diet: Poor dietary habits, often associated with modern industrial food systems and Western diets, are recognized as contributors to a range of health issues, including mental health problems.
- Common Mental Health Conditions: Depression and anxiety are common mental health conditions that have been linked to diet and nutrition. Research in this field aims to understand how specific dietary components can impact these conditions.
- Prevalence and the COVID-19 Pandemic: The prevalence of mental health issues, including depression and anxiety, has not decreased and may have even increased during the COVID-19 pandemic. This has highlighted the need for effective interventions, including nutritional approaches.
- Focus on Evidence-Based Approaches: Nutritional psychiatry is firmly grounded in evidence-based approaches (EBP). It relies on rigorous scientific research to evaluate the impact of various nutrients and dietary patterns on mental health.
- Holistic Perspective: Nutritional psychiatry takes a holistic view of nutrition, recognizing that the effects of food are not limited to just macronutrients and micronutrients. It considers the synergistic interactions of various nutrients, bioactive compounds, and phytochemicals in the diet.
- Applications: Nutritional psychiatry has applications in clinical settings, public health (for prevention and promotion of mental well-being), and policy development to improve mental health outcomes.
- Distinction from Other Approaches: Nutritional psychiatry is distinct from integrative, complementary, alternative, or functional medicine. It does not rely on unproven or unscientific methods but is firmly rooted in the principles of evidence-based medicine and nutrition science.
In practice, nutritional psychiatry may involve interventions such as dietary counseling, nutritional supplementation, or lifestyle changes to improve mental health. For example, specific nutrients like folate and fish oil have been studied for their potential role in managing depression and anxiety. However, the field emphasizes that the overall dietary pattern is crucial and that individual nutrients should be considered in the context of the entire diet.
The emerging field of nutritional psychiatry highlights the importance of a balanced and nutrient-rich diet in promoting good mental health and well-being. It underscores the notion that “you are what you eat” and that food plays a critical role not only in physical health but also in mental and emotional health.

What is the SMILES Project?
The SMILES project, led by Professor Felice Jacka, is a groundbreaking research initiative that focuses on the relationship between diet and mental health. Professor Felice Jacka is a prominent Australian researcher known for her work in nutritional psychiatry. The acronym “SMILES” stands for “Supporting the Modification of lifestyle In Lowered Emotional States.”
Key aspects of the SMILES project include:
- Objective: The primary aim of the SMILES project is to investigate the impact of dietary interventions on individuals with clinical depression. It seeks to determine whether dietary changes can be used as a complementary or alternative treatment approach for depression.
- Clinical Trial: The SMILES project conducted a randomized controlled trial (RCT) to assess the effects of a modified Mediterranean diet on individuals diagnosed with major depressive disorder. The Mediterranean diet is characterized by high consumption of fruits, vegetables, whole grains, legumes, nuts, and healthy fats like olive oil, along with moderate intake of lean proteins, particularly fish.
- Study Design: In the SMILES trial, participants were randomly assigned to either a dietary intervention group or a control group. The dietary intervention group received support and guidance to adopt a modified Mediterranean diet over a 12-week period. The control group did not make any dietary changes.
- Findings: The SMILES project found that individuals in the dietary intervention group who followed the modified Mediterranean diet experienced a significant reduction in their symptoms of depression compared to the control group. This indicated that dietary changes could be an effective way to improve mental health and reduce the severity of depressive symptoms.
- Broader Implications: The findings of the SMILES project have broader implications for the field of nutritional psychiatry. They suggest that dietary interventions could be a valuable part of the treatment approach for mental health conditions, particularly depression.
- Public Health Impact: The research conducted by Professor Felice Jacka and the SMILES project has contributed to the growing body of evidence supporting the role of diet in mental health. It has also influenced public health initiatives and recommendations related to mental health and nutrition.
The SMILES project has been influential in raising awareness of the link between diet and mental health and highlighting the potential of dietary interventions as a part of the holistic approach to treating depression and other mental health disorders. It underscores the importance of considering lifestyle factors, including diet, in the management and prevention of mental health issues.


What should we be eating?
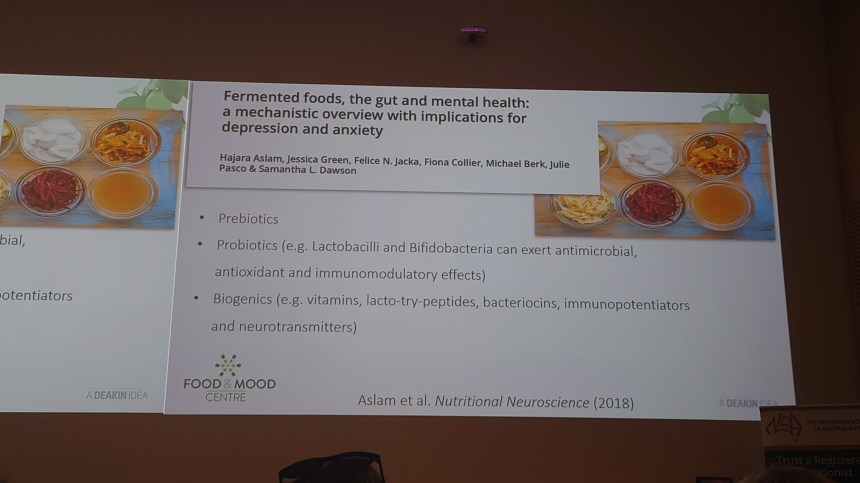
Avoiding ultra-processed foods and incorporating fermented foods into your diet is generally recommended because it can have several positive effects on your gut microbiota and overall health. Here are some reasons why you should consider making this dietary shift:
- Nutrient Density: Ultra-processed foods are typically low in essential nutrients and high in added sugars, unhealthy fats, and additives. In contrast, fermented foods are often rich in essential nutrients and beneficial compounds that support overall health.
- Gut Microbiota Health: Fermented foods contain probiotics, which are beneficial live microorganisms that can positively influence the composition and diversity of your gut microbiota. A diverse and balanced gut microbiota is associated with better health outcomes and a reduced risk of various diseases.
- Probiotics and Prebiotics: Fermented foods provide probiotics, which are “good” bacteria, and some of them also contain prebiotics, which are the non-digestible fibers that nourish the beneficial bacteria in your gut. This combination of probiotics and prebiotics promotes a healthy gut environment.
- Digestive Health: Consuming fermented foods can help improve digestion and reduce gastrointestinal issues. Probiotics can help with conditions such as irritable bowel syndrome (IBS) and diarrhea, while the fiber in some fermented foods supports regular bowel movements.
- Immune System Support: A significant portion of the immune system is located in the gut. By maintaining a balanced gut microbiota through the consumption of fermented foods, you can support your immune system’s function.
- Reduced Inflammation: Some studies suggest that a balanced gut microbiota can help reduce inflammation in the body, which is a common factor in chronic diseases. Fermented foods can contribute to this anti-inflammatory effect.
- Mood and Mental Health: Emerging research indicates that the gut-brain connection is influenced by the gut microbiota. A balanced microbiota is associated with better mental health and a reduced risk of mood disorders, including anxiety and depression.
- Weight Management: A healthier gut microbiota may play a role in weight management. Some studies suggest that people with a more diverse gut microbiota may find it easier to maintain a healthy weight.
- Reduced Risk of Chronic Diseases: A diet rich in ultra-processed foods has been linked to an increased risk of chronic diseases, including heart disease, type 2 diabetes, and obesity. By avoiding these foods and focusing on fermented options, you can reduce this risk.
- Long-Term Health Benefits: Consuming fermented foods is not just a short-term fix but a long-term investment in your health. Regularly including these foods in your diet can provide sustained benefits to your gut microbiota and overall well-being.
Examples of fermented foods to consider adding to your diet include yogurt, kefir, sauerkraut, kimchi, miso, kombucha, and some types of pickles. When choosing these foods, opt for options that are minimally processed and free from excess sugars and additives.
In summary, the choice to avoid ultra-processed foods and consume fermented foods instead is a dietary strategy that can promote a healthier gut microbiota and have a positive impact on various aspects of your health, from digestion to immune function and mental well-being.

How does gut health affect brain health?
Gut health and brain health are intricately connected, and emerging research in the field of neurogastroenterology, also known as the gut-brain axis, sheds light on the profound influence the gut can have on the brain. Here are some of the ways in which gut health can affect brain health:
- Communication via the Vagus Nerve: The vagus nerve is a major communication pathway that connects the gut and the brain. It allows for bidirectional communication, with signals traveling from the gut to the brain and vice versa. This means that the health and state of the gut can influence the brain’s function and vice versa.
- Microbiota-Brain Interaction: The gut is home to trillions of microorganisms, collectively known as the gut microbiota. This microbiota plays a crucial role in digestion, nutrient absorption, and immune system regulation. Recent studies have shown that the gut microbiota can also influence brain function. For example, the gut microbiota can produce neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), which can impact mood and behavior.
- Immune System Regulation: A significant portion of the body’s immune cells resides in the gut. An imbalanced or inflamed gut can lead to systemic inflammation, which is associated with various brain disorders, including depression and neurodegenerative diseases.
- Influence on Mood and Mental Health: Studies have found a strong connection between gut health and mental health. An unhealthy gut can contribute to mood disorders such as anxiety and depression. This is partly due to the production of neurotransmitters in the gut and the role of the gut microbiota in regulating inflammation.
- Neurotransmitter Production: The gut microbiota can synthesize and modulate the levels of certain neurotransmitters, which are chemical messengers in the brain that affect mood, cognition, and behavior. For example, serotonin, often called the “feel-good” neurotransmitter, is produced in the gut. An imbalanced gut microbiota can impact serotonin levels and mood.
- Influence on Cognitive Function: Some research suggests that gut health can influence cognitive function and the risk of neurodegenerative diseases. An unhealthy gut may be associated with a higher risk of conditions like Alzheimer’s disease.
- Stress Response: The gut-brain axis is involved in the body’s response to stress. Chronic stress can negatively affect gut health, and an imbalanced gut can, in turn, contribute to stress and anxiety. This creates a feedback loop that can be detrimental to both gut and brain health.
- Effects of Diet: Diet plays a crucial role in gut health and, by extension, brain health. Diets high in ultra-processed foods and low in fiber can disrupt the gut microbiota and contribute to inflammation. In contrast, a diet rich in fiber, antioxidants, and fermented foods can support gut health and positively influence the brain.
In summary, gut health has a profound impact on brain health and overall well-being. The gut-brain axis is a complex and dynamic system that involves communication between the gut, the gut microbiota, and the brain. Prioritizing a diet that supports a healthy gut, managing stress, and addressing gut-related issues can have positive effects on mood, cognition, and overall mental health.
References
About the SMILES Project https://foodandmoodcentre.com.au/smiles-trial/
What is Nutritional Psychiatry https://foodandmoodcentre.com.au/2017/10/nutritional-psychiatry-investigating-the-link-between-food-and-mood/
Introduction to Nutritional Psychiatry with Professor Felice Jacka and Doctor Tetyana Rocks https://impact.deakin.edu.au/2022/09/introduction-to-nutritional-psychiatry-nutri-psyche/


I wish this got more attention. I’ve been following this area of research for years. Right before COVID19, I unintentionally cured decades of depression when I changed my diet to lose weight. And I’ve kept it off ever since. Have you read Chris Palmer’s Brain Energy, Geogia Ede’s Change Your Diet, Change Your Mind, and Bret Scher’s work?
LikeLike